Unraveling the complexities of medical billing? Examples of calculating the patient and insurance portion of charges offer a straightforward path to understanding how costs are allocated. This comprehensive guide simplifies the often-confusing process, providing clear explanations and real-world examples to empower you with the knowledge to navigate these calculations with confidence.
From understanding different insurance plan types to mastering the various calculation methods, this resource equips you with the tools to accurately determine the patient’s and insurance company’s responsibilities. The examples will illustrate how co-pays, co-insurance, and deductibles affect the final cost, ultimately leading to a more transparent and manageable healthcare experience.
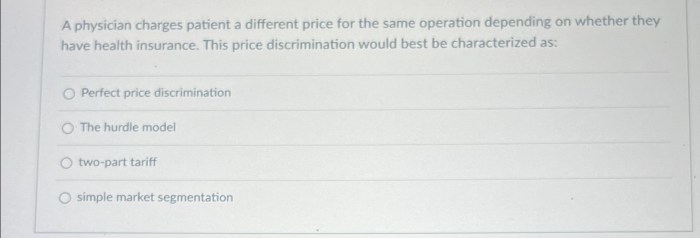
Introduction to Patient and Insurance Charge Calculations
Hey there, future billing wizards! Navigating the world of medical billing can feel like deciphering ancient hieroglyphics sometimes. But fear not, grasshopper! We’re about to demystify the process of figuring out who foots the bill for your medical services. It’s all about calculating patient and insurance responsibilities, and we’ll break it down like a delicious, easy-to-digest meal.This process isn’t just a matter of math; it’s a complex dance between medical providers, insurance companies, and patients.
Understanding the different factors at play is key to avoiding surprises and ensuring everyone’s on the same page. Let’s dive in!
Factors Influencing Charge Calculations
Various factors impact the amount each party owes. Think of it as a recipe, where each ingredient plays a vital role in determining the final dish. Insurance plans, for instance, have different structures and benefits. The type of service rendered, the patient’s health status, and the specific medical facility all affect the cost breakdown. Each scenario requires a personalized approach.
Common Terminology
Knowing the lingo is crucial. Here’s a quick glossary to help you navigate the world of medical billing:
- Copay: A fixed amount a patient pays for a covered service, like a visit to the doctor or a prescription. Imagine it as a small toll to enter the healthcare highway.
- Coinsurance: A percentage of the cost of a covered service that a patient pays after meeting the deductible. It’s like a shared responsibility between the patient and insurance company.
- Deductible: The amount a patient must pay out-of-pocket for covered services before the insurance company starts paying. Think of it as a hurdle you have to clear before the insurance company kicks in.
- Network: A list of healthcare providers who have agreements with an insurance company to provide services at a discounted rate. This means you might have to pay less if you see a doctor in their network.
Calculating Patient and Insurance Responsibility
Let’s illustrate with a simple example. Imagine a patient with a $1,000 office visit. Their insurance plan has a $1,500 deductible and 20% coinsurance.
| Item | Amount |
|---|---|
| Office Visit | $1,000 |
| Deductible | $1,500 |
| Coinsurance | $200 |
| Patient’s Responsibility | $800 |
Note: This is a simplified example. Real-world calculations can be more complex, depending on specific plan details and services rendered. Always check with your insurance provider for the most accurate information.
This table clearly displays the calculated amounts. Patient’s responsibility will differ depending on factors like the specific service, whether or not the provider is in network, and how the insurance policy structures the coverage.
Types of Insurance Plans and Their Impact
Insurance plans, oh boy, they’re like different flavors of ice cream – each one with its own unique set of perks and drawbacks. Understanding these plans is key to figuring out who foots the bill for what. Some plans are generous, others are stingy, and some are just plain confusing. Let’s dive in!Different insurance plans have different rules for who pays what.
It’s a bit like a game of charades, where the insurance company acts out how much they’ll cover. Knowing the rules of the game will help you avoid getting stuck with an unexpected bill.
Health Maintenance Organizations (HMOs)
HMOs are like a tightly knit community. They’re great for routine care, but specialty care can be a bit of a hassle. Think of it as a neighborhood clinic. You pick a primary care physician (PCP) within the network, and they’re your gatekeeper for other specialists. If you want to see a cardiologist, your PCP has to give you a referral.
This gatekeeping system helps control costs. But if you want a different doctor outside the network, you’re on your own. You often pay a monthly fee (premium) and a copay for each visit.
Preferred Provider Organizations (PPOs)
PPOs are like a more open-door policy. You have more flexibility in choosing doctors, both inside and outside the network. You might pay a higher premium, but you don’t need a referral to see a specialist. However, the cost for doctors outside the network is usually higher. You might pay a higher copay for a doctor outside the network, but you have more options.
Point-of-Service (POS) Plans
POS plans are a hybrid, combining aspects of HMOs and PPOs. You pick a PCP, but you have more freedom than with an HMO. You can see doctors outside the network, but it’ll likely cost you more. POS plans are a bit like a buffet – you have more choices, but some options are more expensive. Think of it as a mix-and-match approach to care.
They generally require pre-authorization for certain procedures, just like HMOs.
Impact on Patient and Insurance Share of Costs
| Plan Type | Patient’s Share (Generally) | Insurance’s Share (Generally) | Flexibility |
|---|---|---|---|
| HMO | Lower premiums, higher co-pays and deductibles for out-of-network care. | Lower premiums for in-network care. | Limited flexibility, requires referral from PCP. |
| PPO | Higher premiums, lower co-pays and deductibles for both in-network and out-of-network care. | Higher premiums for broader coverage. | More flexibility, no referral required for out-of-network care. |
| POS | Lower premiums than PPOs but higher than HMOs, and co-pays/deductibles vary depending on in- or out-of-network care. | Moderate premiums. | Moderate flexibility. |
Role of Pre-authorization and Referrals
Pre-authorization and referrals are like permission slips. They ensure that the insurance company approves the care before it’s provided, especially for costly procedures. HMOs often require pre-authorization and referrals for most services, to help control costs. PPOs might have pre-authorization requirements for some complex procedures, but they are usually less strict.
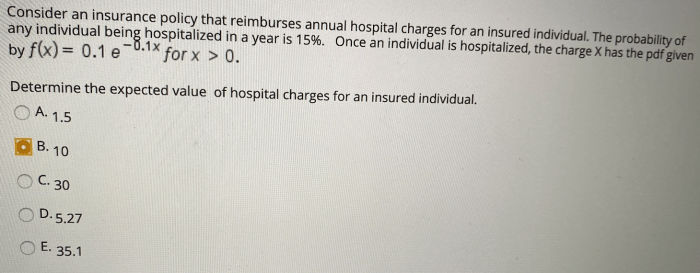
Common Calculation Methods
Calculating patient responsibility can feel like deciphering a secret code, but fear not, fellow healthcare heroes! Understanding the standard methods used makes it much easier to figure out how much the patient owes. We’ll break down the common approaches, complete with examples, so you can confidently calculate patient responsibility.Calculating patient responsibility isn’t rocket science, but it’s crucial to get it right.
Knowing the specific insurance plan details is key, as different plans have different rules about what’s covered. This section will cover the common methods and show you how to apply them.
So, like, calculating patient and insurance costs is kinda a big deal, right? It’s all about figuring out how much each party owes. You gotta look at the total bill, then see what the insurance will cover. Finding a sweet spot for Lakeview Terrace Apartments Augusta GA is important too, you know? Lakeview Terrace Apartments Augusta GA has some pretty cool digs.
Anyway, after that, you basically just subtract what insurance covers from the total, and whatever’s left is the patient’s responsibility. Pretty straightforward, tbh.
Standard Methods for Calculating Patient Responsibility
Different insurance plans use different methods to calculate the patient’s portion of healthcare costs. These methods, while varied, generally follow a predictable structure. Understanding these structures is essential for accurate billing.
- Copay-based Calculations: This is the simplest method. The patient pays a fixed amount (the copay) for each visit or service. For example, a plan might have a $25 copay for a doctor’s visit. The patient pays the copay regardless of the total cost of the visit. This straightforward approach is popular because it’s easy to understand and apply.
- Coinsurance-based Calculations: Coinsurance is a percentage of the cost that the patient pays. If a plan has 20% coinsurance, the patient pays 20% of the cost of the service after the deductible has been met. Imagine a $1000 procedure; with 20% coinsurance, the patient would pay $200. This is a more complex calculation than a copay but is still straightforward.
- Deductible-based Calculations: A deductible is the amount the patient must pay out-of-pocket before the insurance company starts covering costs. For instance, a deductible of $1,500 means the patient must pay the first $1,500 of medical expenses before insurance kicks in. The patient’s responsibility will be the deductible amount plus any applicable copays or coinsurance, once the deductible is met.
This is a crucial element to factor in, as it affects how much the patient will pay.
Example Scenarios
Let’s look at some real-world examples to illustrate these concepts.
| Scenario | Plan Details | Patient Responsibility |
|---|---|---|
| Doctor’s visit | $25 copay, no deductible, 20% coinsurance | If the total bill is $150, the patient pays $25 (copay) + 20% of the remaining cost. |
| Hospital stay | $2,000 deductible, 80% coinsurance, $50 copay per day | The patient pays the deductible first, then 20% of the cost of the stay after the deductible is met. If the total cost is $5,000 and the stay is for 5 days, the patient pays $2,000 (deductible) + ($50/day
|
Step-by-Step Procedure for Calculating Patient’s Portion
Imagine a patient with a specific plan:
A $1000 deductible, 20% coinsurance, and $25 copay for a specialist visit. The total bill is $2500.
- Deductible Application: The patient’s $1000 deductible is met first.
- Copay Calculation: The $25 copay is added to the total.
- Coinsurance Calculation: 20% of the remaining amount ($2500 – $1000 – $25 = $1475) is calculated, which is $295.
- Total Patient Responsibility: $1000 (deductible) + $25 (copay) + $295 (coinsurance) = $1320.
Handling Different Scenarios and Exceptions
Okay, so we’ve covered the basics of calculating patient and insurance portions. But what happens when things get a little…extra*? Like, a sudden catastrophic illness or a provider who’s not in the insurance network? Let’s dive into those tricky situations.Dealing with unusual circumstances requires a well-defined procedure. We need to ensure fairness and accuracy, especially when dealing with potentially life-altering events or unexpected medical situations.
Navigating these exceptions requires a systematic approach to avoid costly errors and maintain patient trust.
Catastrophic Illnesses
Catastrophic illnesses often require extensive and costly care. Standard calculations might not fully cover the necessary expenses. These cases demand a flexible approach, considering the unique financial needs of the patient. Negotiating with the insurance company is crucial, often involving pre-authorization or case management to ensure the patient receives necessary care without facing overwhelming financial burdens. The insurance company might have specific guidelines for approving extraordinary care or potentially provide higher coverage limits in these situations.
Proper documentation and communication with the insurance company are key to securing the necessary approvals and payments.
Out-of-Network Providers
Out-of-network providers present another challenge. Their fees are often higher than in-network rates. Insurance companies typically pay a lower amount for services rendered by out-of-network providers, and sometimes they might not cover the entire cost. Understanding the specific rules of the insurance plan is essential. This often involves determining the patient’s responsibility, which is typically the difference between the out-of-network provider’s charges and the amount the insurance company will pay.
Thorough communication with both the patient and the insurance company is vital to ensure clarity and prevent misunderstandings.
Appeals and Disputes, Examples of calculating the patient and insurance portion of charges
“Disputes are handled through a well-defined appeals process. A thorough explanation of the reason for the denial or reduction of payment is crucial.”
Disagreements on charges can arise. Perhaps the insurance company denies a claim or reduces the payment amount. A well-defined appeals process exists to address such disputes. These procedures usually involve submitting supporting documentation and following specific steps Artikeld by the insurance company. Clear and concise communication with the insurance company is essential throughout the appeal process.
Sometimes, a neutral third party mediator might be involved to help reach a mutually agreeable solution. A thorough understanding of the appeals process, and timely action, is crucial for resolving disagreements fairly.
Scenario-Specific Actions
| Scenario | Action |
|---|---|
| Catastrophic illness | Pre-authorization, case management, negotiating with insurance company. |
| Out-of-network provider | Determine patient responsibility (difference between provider’s fee and insurance payment). Communicate with patient and insurance company. |
| Insurance claim denial/reduction | Submit supporting documentation, follow insurance company’s appeals process, and seek mediation if necessary. |
Illustrative Examples of Calculations
Alright, buckle up buttercups! Let’s dive into some real-world scenarios for calculating patient and insurance responsibilities. Imagine trying to decipher a medical bill without a cheat sheet – it’s like trying to solve a complex puzzle with missing pieces. These examples will help you visualize the process and understand the various insurance plan types.These examples showcase how different insurance plans impact the final bill.
We’ll break down the calculations step-by-step, making it easier to understand the complexities. We’re talking about deductibles, co-pays, co-insurance, and all the other fun stuff. Let’s get started!
Example 1: The Basic Bronze Plan
This scenario illustrates a patient with a Bronze plan, which is a relatively common plan type. The patient’s total bill is $500, and the insurance plan has a $1,500 deductible. The co-insurance percentage is 80%.
- The patient’s responsibility is calculated after the deductible is met.
- Since the deductible is higher than the bill, the patient’s responsibility is determined by the co-insurance rate.
- The insurance company pays 80% of the $500 bill.
- 20% of the bill, $100, is the patient’s responsibility.
Example 2: The Generous Silver Plan
Let’s say our patient has a Silver plan. This example shows how a different plan structure leads to different results. The total bill is $1000, and the insurance plan has a $1,000 deductible and 80% co-insurance.
- The patient has already met their deductible of $1000.
- The insurance company pays 80% of the $1000 bill, which is $800.
- The patient’s responsibility is $200, which is 20% of the bill.
Example 3: The Premium Platinum Plan
Our final example is a Platinum plan. These plans usually offer the most comprehensive coverage. The total bill is $2000. The patient’s deductible is $2000, and co-insurance is 20%.
- The patient hasn’t met their deductible, so they are responsible for the entire $2000 bill.
Example 4: The Catastrophic Gold Plan
Now let’s say our patient has a Gold plan. It’s an expensive plan, but it’s the most extensive. The total bill is $3000. The deductible is $5000 and the co-insurance is 50%.
- The patient has not yet met their deductible, so the entire $3000 bill is the patient’s responsibility.
Calculation Breakdown Table
| Example | Plan Type | Total Bill | Deductible | Co-insurance (%) | Insurance Payment | Patient Responsibility |
|---|---|---|---|---|---|---|
| 1 | Bronze | $500 | $1500 | 80% | $400 | $100 |
| 2 | Silver | $1000 | $1000 | 80% | $800 | $200 |
| 3 | Platinum | $2000 | $2000 | 20% | $1600 | $400 |
| 4 | Gold | $3000 | $5000 | 50% | $0 | $3000 |
Illustrative Examples with Images
Hey there, future billing wizards! Let’s dive into some real-world examples of calculating patient and insurance responsibilities. Forget those confusing spreadsheets – we’re going visual! This will make the whole process crystal clear.Visual aids are key to understanding complex financial calculations. Instead of just numbers on a page, we’ll use diagrams and charts to show you exactly how the calculations work and where the numbers come from.
So, like, calculating patient and insurance costs is kinda a big deal, right? Think about all those forms and stuff. It’s like, totally figuring out how much the insurance company is gonna pay, and how much you owe. Plus, you know, Atlanta United vs FC Cincinnati? That game’s gonna be a total blast! atlanta united vs fc cincinnati is gonna be epic.
Anyway, back to the charges, you gotta know the specifics for the different types of procedures, right? Gotta get that down pat!
This visual approach helps track the flow of information, making the whole process easier to digest.
Patient Responsibility Calculation Example
This example shows a simplified scenario. Imagine a patient named Barry with a $500 bill for a procedure. His insurance plan covers 80% of the charges. 
The diagram would visually represent the calculation steps. A rectangle could represent Barry’s total bill, divided into two parts: insurance coverage and patient responsibility. The insurance coverage portion would be 80% of $500, and the patient responsibility portion would be the remaining 20%. Clear labels are essential for understanding.
Insurance Claim Process Flowchart
This flowchart demonstrates the typical journey of an insurance claim. 
This flowchart should visually depict the steps, from the doctor submitting the claim to the insurance company processing it and sending the payment. Key steps might include claim submission, claim review, pre-authorization, payment processing, and the eventual notification to the patient and provider about the insurance portion of the bill.
In-Network vs. Out-of-Network Charges
This graphic visually compares in-network and out-of-network charges. 
The graphic would have two columns, one for in-network and one for out-of-network charges. In-network charges would be lower because the provider has a contract with the insurance company. Out-of-network charges would be higher, as the insurance company typically pays less. The diagram should clearly indicate the percentage covered by insurance in each scenario.
Visual Representation of Calculation Procedures
Figuring out who pays what for medical bills can be a real headache, right? It’s like trying to solve a complex puzzle with different pieces, each representing a different insurance plan and the patient’s responsibility. Luckily, flowcharts can be our friendly guides, making these calculations a bit more straightforward.Flowcharts visually represent the steps involved in any process, making it easy to follow the logic and identify potential pitfalls.
They’re like a roadmap, showing you the path to the correct answer, whether it’s the patient’s or the insurance company’s share of the bill.
Patient’s Portion Calculation Flowchart
This flowchart will guide you through the process of calculating the patient’s portion of a medical bill. Understanding this is crucial for both patients and healthcare providers, as it clarifies the financial obligations involved.
The flowchart begins with gathering the total charges for the services rendered. Then, the applicable insurance plan is identified, and its coverage details are accessed. Crucially, deductibles and co-pays are calculated based on the plan’s stipulations. Next, the portion covered by insurance is subtracted from the total charges to arrive at the remaining balance. This remaining balance is the patient’s responsibility.
The final step is presenting the patient with a clear breakdown of the charges, the insurance coverage, and their outstanding balance.
Insurance Company’s Responsibility Calculation Flowchart
Understanding the insurance company’s responsibility in covering medical bills is equally important. This flowchart illustrates the process.
The flowchart starts by determining the total charges for the services rendered. Next, the insurance plan details are accessed to determine the coverage limits. Co-pays and deductibles are calculated, and the applicable portion of the total charges is calculated based on the plan’s benefits. The flowchart concludes by documenting the amount the insurance company will pay, providing a clear record of their financial commitment.
Example Scenario
Let’s say a patient has a $1,000 bill for a procedure. Their insurance plan has a $500 deductible and a 20% co-insurance rate. Following the flowchart, the insurance company would pay $800 (100%
- 20% = 80% of the charges, which is 80%
- $1,000 = $800). The patient’s portion would be $200 (100%
- 80% = 20% of the charges, which is 20%
- $1,000 = $200).
Epilogue: Examples Of Calculating The Patient And Insurance Portion Of Charges
In conclusion, accurately calculating patient and insurance responsibility for medical charges is crucial for both patients and healthcare providers. This guide offers a structured approach to understanding the process, equipping you with the knowledge to navigate various scenarios and ensuring clarity and transparency in the billing process. Armed with these examples, you’ll feel confident and empowered to handle medical expenses with ease.
Key Questions Answered
What if my insurance plan is out-of-network?
Out-of-network charges are often significantly higher than in-network costs. The patient’s responsibility typically increases, and the insurance company’s payment may be limited or nonexistent. The specific calculation depends on the plan’s details. Consulting with the insurance provider is recommended for clarification.
How are appeals handled regarding billing discrepancies?
Each insurance company has a specific appeals process. Typically, patients must submit a written appeal outlining the reason for the dispute. Supporting documentation, such as medical records or provider correspondence, is crucial. Following the insurance company’s guidelines for appeal procedures is essential for a successful outcome.
What is the difference between a co-pay and co-insurance?
A co-pay is a fixed amount paid by the patient each time a service is used. Co-insurance is a percentage of the cost that the patient is responsible for after meeting the deductible. Understanding these distinctions is key to accurately calculating your share of medical expenses.
What are some common factors that influence the calculation of patient responsibility?
Several factors influence patient responsibility, including the type of insurance plan, the provider’s network status, co-pays, co-insurance, deductibles, and out-of-pocket maximums. Each factor can significantly impact the final amount owed by the patient.
